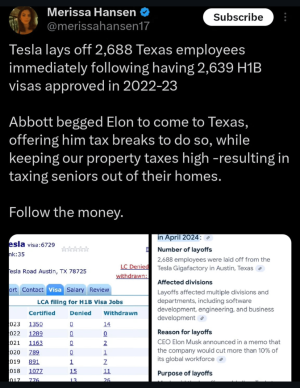
As someone who works in Healthcare and for one of the companies listed, that chart can be a bit misleading. Claims mostly get denied for things like a provider billing error in which the provider often times is asked to rebill. In cases when a service is denied because it's not covered by cms, or the states Medicaid programs, contracted providers are not to bill the patient per their contract with the healthplan. They are supposed to "eat" that loss. Unfortunately, a lot of members don't know this information and don't report this to their Healthcare provider that they have been billed.
Btw.. I am in no way defending greedy Healthcare organizations.
Appreciate the insight but that still doesn't change the fact that uniteds rate is so much higher. You have to assume that across the board, the amount of billing errors or programs denied by state programs should be a more or less evenly distributed. So if United is denying at a much higher rate than most others, it's because there's something in their process or philosophy that's causing their rejection rate to be so high.