- 9,634
- 6,434
- Joined
- Sep 17, 2006
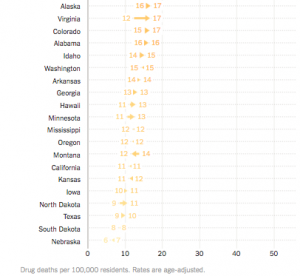
I’ve seen one of my closest friends who had the most potential out of all of our crew lose it all over pills.
Strongest dude I knew but couldn’t beat those inner demons.
Strongest dude I knew but couldn’t beat those inner demons.